So, finally the heart results have come back. If you haven’t been keeping up with all of my latest and greatest developments in the slow-moving train wreck that is called systemic sclerosis, let me quickly catch you up.
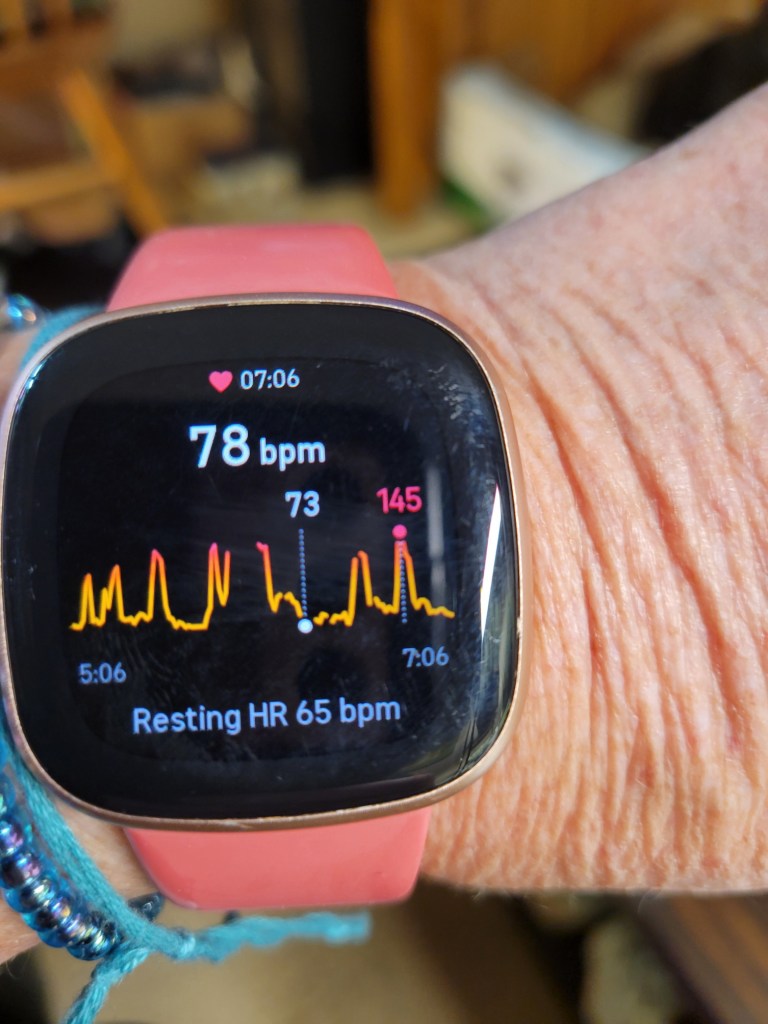
Over the summer I started to notice that my Fitbit was alarming frequently because my heartbeat was high. My heartrate was jumping suddenly from a moderate mid-70s bpm to over 140 bpm: cue the panting! I’d have to stop whatever I was doing to lean over while I caught my breath, and then it would be over. Sometimes my chest hurt, and I was pretty sure that this was contributing to my fatigue.

I do have a long history of shortness of breath, and I’ve been diagnosed with several heart and lung issues that explained my symptoms: pulmonary hypertension, cardiac fibrosis, fluid around my heart, lung disease, and… yeah. I’ve been short of breath like this for a long time and I’ve just been dealing with it as my new normal. Still, the Fitbit was new data, so I sent an email to my cardiologist, and he ordered up a 30-day heart monitor test.

Tuesday afternoon the results were in, and my cardiologist contacted me with the results. It’s kind of a good news/good news/bad news diagnosis. I have a type of supraventricular tachycardia called paroxysmal atrial tachycardia (called PAT for short). I had to do some google searches to understand those crazy terms. The commonsense translation would be: sudden onset rapid beating of my heart’s upper chamber (the atrium). In even more simple terms, my heart rhythm slips out of control suddenly and the upper chamber is beating waaay too fast. Here’s the good news: this is a pretty benign heart rhythm issue (no blood clots, heart attacks or strokes here!!), and it can be treated (probably). The bad news is… I’m stuck with it, and it is pretty unpredictable. The other bad news is that I should go on oxygen more often in the daytime as PAT episodes seem to be triggered when my oxygen levels drop. That’s why it hits when I’m folding laundry, or right after coming up the stairs, or when I rush to the door to answer the doorbell…

Why wait on a new drug? Well… I’m just now recovering from a pretty bad flare that hit my tendons, wrists and knees with paroxysmal fury. Paroxysmal is a great word, don’t you think? What is really crazy, my heart symptoms improved while I was down with the flare, making me wonder if the two are somehow connected. I want to wait to start a new medication until after my rheumatologist has a chance to sort out what is happening with my poor wrists and knees. I am suspicious about calcium being involved somehow, and the treatment for PAT involves calcium channel blockers. There may be no connection if there are different pathways involved, but still… calcium is the multi-headed monster of the moment with new calcium deposits appearing on my arms and legs, osteoporosis, and a previously floated notion that I might have pseudogout (which is caused by calcium pyrophosphate crystals in joints… wrists and knees being hit the worst… and my knee x-rays showed that I had calcium deposits in the tissue around my knee…). My cardiologist is okay with a delay in treatment with the understanding that I need to contact him if things get worse.
I just love my doctors!
So, here is the lesson from this adventure. Data really changes a conversation. Having that picture of my Fitbit made a huge difference; after months of explaining that I had sudden shortness of breath things changed with the one email and attached photo. The results of the heart monitor test have now returned a data-driven diagnosis that helps me understand what is happening and makes treatment possible. It is helpful to email your doctors (instead of making phone calls…) as you have a clear record of your interaction. Google with abandon!! Rely on the advice of your doctors; they went to medical school after all, but try to be an active partner in your treatment plan.
Dang. There is another diagnosis on that growing list… no one will believe me so we should just keep this quiet. Paroxysmal Atrial Tachycardia.
Postscript: I forgot to mention, that of the three types of supraventricular tachycardia, PAT is the one that is the least common. Figures. Once a zebra, always a zebra!!

I have to “like” your post, Marilyn, because I recognize quite a bit. I have very recently been discussing my paroxysmal atrial fibrillation with a new young GP (whom I had hoped might turn out to become my regular GP, but no dice). And my case of hypercalcemia – the seriousness or lack of same being quite unknown to me, as neither the cardio I briefly had nor the GP I’ve been attending for some years has ever seen fit to tell me exactly what is going on. And I have nothing like your understanding of your condition/s. A very old friend visited me a couple of weeks ago, from Sydney; and she was infuriated with me for being so passive about it all: “You must tell them you want your own copy of the results of every test they send you for !” she reprimanded me; “and you must tell them to explain whatever you don’t understand !”
When I reflect upon how your excellent brain – trained for learning and teaching – has supported you in every new and wondrous discovery about your body’s shenanigans, I am indeed ashamed. 😦 I believe this lack of attention is due to the fact that until a year or two ago, there was (apparently) nothing at all wrong with my health; and I find it challenging to have to become a “patient with conditions” at my age.
You were once much the same – fancy-free and able to live life as you wished. And now, with the crowding in of the things affecting you, you do not turn away and pretend there’s nothing going on but put your head down and FIND OUT.
Would you believe that there’s something about your ailments that makes you luckier than I ? – it is that you’re in a position to accept everything your doctors pronounce, or ascertain where they’re wrong.
I, on the contrary, do not believe in the fear of cholesterol that’s the basis of what all the GPs/cardios down here have been taught; so I start out from the position of not accepting what they claim is going on. Difficult. And my brain isn’t good enough to be able to explain my position in detail.
Oh dear. You missed the years where I was pretty passive and dependent on my doctors, ignoring some pretty big red flags, and without any of my test results. I think that it is part of the grief process that comes when, as you said, you transition from a healthy person hiking mountains, to a person with symptoms, and then a person with a diagnosis. It is a hard, difficult transition to accept that things are changing because it requires that your entire sense of self needs to alter.
So, I had to learn to pull myself together, remind myself who I was, and get test results, read up on my conditions, fire some doctors, and finally secure the help that I needed. The Medical Gaslighting was strong with some of those guys that I kicked to the curb.
When you are ready to deal with it, you will get those copies of test results. You too are strong and talented, and when you are ready, you will put your head down, find out about what is happening, and then deal with it!!
Hugs!
My goodness, but you’re a generous soul !!!
I forgot to mention that I am also, as you said, lucky that I have a lot going for me. Like, much more than the usual patient with my diagnosis. Molecular biology degree, years in an immunology research lab, then the years teaching biology. I had the good luck to work for the school district training other teachers and facilitating working committees (my superpower) that helped me learn how to listen carefully, write well, and then communicate effectively with the powers-that-be. All of that now comes to my aid as I deal with this chapter of my life.
And you deal with it with grace. And your brains.
If you had to have a cardiovascular problem, at least PAT’s a benign one, thank heaven. However benign, though, it’s rough to be short of breath when the galloping paroxysms occur. You’re amazing to take this new turn of events in your stride by looking at the positive aspects of that syndrome: it doesn’t herald blood clots, heart attacks, or strokes.
I love the picture of your mild-appearing ornamental gargoyles standing guard above the fray. If they were more ferocious looking and their mouths open, they could almost make it as downspouts attached to Notre Dame or some other medieval cathedral.
I think that I am desensitized to some degree at this point. I was a little hesitant to start a new drug two years ago because it carried an increased risk for heart attack. I had to sign off on paperwork acknowledging that I was aware of the risk! I bought a medical bracelet because I can’t have nitrates (and if something happened, you know the paramedics would administer nitro…) and took the drug. After that, everything seems less serious.
The cats sometimes startle me when I glance up and see them on overwatch. It’s even more alarming if I wake up to find them up there! I suspect they are watching bugs, but still…
Not to mention it’s warmer up near the ceiling.
Thank goodness this has some positive result – and for your intelligence and determination to be an active partner with your docs.
I am very happy with my docs being okay with including me in decision making. Well, I would look for new ones if they didn’t, but still…
I agree. I figure my docs and I are partners in whatever is going on. They might hate it (I’m a doctor’s kid. Can’t help it.) but if they don’t consider me an equal partner, I’ll find other doctors.
Exactly. If they are dismissive or talk down to me, I move on.
Good advice about trying to get data to get doctor’s to treat the issue. Do you have an oxygen monitor to help you decide when you need to be “hooked up”? On the positive side, sounds like there is action you can do to help with the symptoms.
I do have a pulse oximeter that measures my oxygen levels, and lately I bought another smart watch cheap that checks it at my wrist. There are more expensive devices for sale, but so far I haven’t gotten anything.
I really watch the barometric pressure as it impacts my oxygen levels, and also hot weather is a problem. Love my oxygen machine on those days.
OMG, you are amazing!!! You are an inspiration.
[takes a small, very small curtsey]
I like to believe that adversity reveals who people really are, and I’m just trying to be the person my cats think I am. 🙂
Interesting. I didn’t know barometric pressure impacts one’s oxygen levels. I did buy a pulse oximeter when covid started, and my smart watch measures it too if I put it high enough on my wrist (where I don’t like to wear it).
That heart monitor is pretty slick. Some decades ago when my brother wore one for a while, it was some bulky thing that he had to have strapped around his chest. Probably pretty uncomfortable.
Yep, 147 bpm would definitely get my attention. Pretty cool that smart watches can monitor so much. And smartphones. I do skip the snore detection, though. Phone can’t hear it with my sound machine playing a thunderstorm all night.
I have a vision of you marching into a multispecialty clinic with all the different specialists lined up to meet you. I’m just so glad you have a bunch of doctors you really like and trust. It makes all the difference, doesn’t it? And it’s something too many people don’t have.
Pet those kitties for me.
I had to do some google searching to understand the barometric pressure phenomenon when I realized it was happening to me. In short, when the pressure drops, tissue expands and that sets off an inflammatory cascade of molecules that interact with the immune system. The most obvious sign of dropping pressure is painful joints, but it can become systemic as the cytokines circulate and impact other tissues like lungs. I guess it can even trigger asthma attacks! My sister and I now utilize air pressure trackers that forecast a few days out so we can plan our trips out of the house.
I know several other patients who have gone to multispecialty clinics (like Mayo) and I kind of think that what I’m getting is pretty comparable. I’m a Kaiser patient, and I’m seeing doctors who are based at the big downtown facility that is connected to St. Joe’s, and a couple of them are really highly regarded doctors and I am sooo lucky to have them. The main team all know each other and have created a multidisciplinary treatment plan that is collaborative in the decision making. They loop my primary care doc into all the email traffic, and I see her to go over all the test results together and then she plugs the gaps. I’m really comfortable with how things are going with these guys!
I’ve not usually paid much attention to my Fitbit heart monitoring but it did tell me this week my Heart Beat Variability dropped from 33 to 16 this week ‘which may indicate signs of stress, strain or illness’. So my heartbreak over losing our dog is literally physical. These Fitbit sensors are pretty clever bits of tech and I’m glad they were evidence to show your doctor.
Oh, how sad. Even your Fitbit knows what heartbreak looks like. 😦 I have found mine to be really useful in other ways; early on in my shortness of breath and fatigue journey doctors kept telling me that I had sleep apnea (even when testing said that I didn’t). I kept pushing back, saying that my Fitbit showed that I not only didn’t I wake up very often during the night, but I was sleeping so deeply that my sleep animal is the bear (as in… I’m hibernating!!). The recent heart monitor results really backed that up… my heartrate goes into the 40s while I am sleeping, so I also have bradycardia. The Fitbit data really empowered me to keep pushing the doctors to consider other causes for my symptoms, and eventually they got to pulmonary hypertension and now, tachycardia. Data is power!!
I am so sorry this is another thing on the pile you are dealing with, but YAY for some hard data! At least it has helped with providing some clarification.
One of my doctors early on told me that it is good to have a diagnosis, even if it is a shame. In this case, I’m so glad that I finally have a name for the extreme, sudden shortness of breath, and it is treatable, and not life-threatening.
True. It’s a place to start figuring things out if nothing else.
PAT sounds like a rubbish friend, who invited her to the party?? I’m glad it’s not super-serious and won’t cause any worse problems.